Abstract
Background
There is limited experimental evidence on transitional care interventions beyond 30 days post-discharge and in vulnerable populations.
Objective
Evaluate effects of a transitional care practice (TC) that comprehensively addresses patients’ medical and psychosocial needs following hospital discharge.
Design
Pragmatic, randomized comparative effectiveness trial.
Patients
Adults discharged from an initial emergency, observation, or inpatient hospital encounter with no trusted usual source of care.
Interventions
TC intervention included a scheduled post-discharge appointment at the TC practice, where a multidisciplinary team comprehensively assessed patients’ medical and psychosocial needs, addressed modifiable barriers, and subsequent linkage to a new primary care source. Routine Care involved assistance scheduling a post-discharge appointment with a primary care provider that often partnered with the hospital where the initial encounter occurred.
Main Measures
The primary outcome was a binary indicator of death or additional hospital encounters within 90 days of initial discharge. Secondary outcomes included any additional hospital encounters, and counts of hospital encounters, over 180 days.
Key Results
Four hundred ninety patients were randomized to TC intervention and 164 to Routine Care; 34.6% were uninsured, 49.7% had Medicaid, and 57.4% were homeless or lived in a high-poverty area. There was no significant difference between arms in the 90-day probability of death or additional hospital encounters (relative risk [RR] 0.89; 0.91; 95% confidence interval [CI] 0.74–1.13). However, TC patients had 37% and 35% lower probability of any inpatient admission over 90 days (RR 0.63; 95% CI 0.43–0.91) and 180 days (RR 0.65; 95% CI 0.47–0.89), respectively. Over 180 days, TC patients had 42% fewer inpatient admissions (incidence rate ratio 0.58; 95% CI 0.37–0.90).
Conclusions
Among patients randomized to a patient-centered transitional care intervention, there was no significant reduction in 90-day probability of death or additional hospital encounters. However, there were significant decreases in measures of inpatient admissions over 180 days.
Trial Registration
clinicaltrials.gov identifier NCT03066492.
Similar content being viewed by others
INTRODUCTION
Care transitions following hospital discharge are often characterized by lack of timely follow-up,1 failure to address psychosocial factors related to hospitalization,2 and poor communication of care plans to patients and follow-up providers.3, 4 These issues are particularly salient for vulnerable populations such as patients of low socioeconomic status (SES), who face challenges such as understanding and executing discharge plans, competing socioeconomic needs, and poor access and engagement with outpatient providers.5,6,7
There is very limited evidence of transitional care interventions that reduce rehospitalization in vulnerable populations. Although a reengineered safety-net hospital discharge program reduced 30-day hospital encounters by 30%,8 other randomized trials with large proportions of low SES patients reported no reductions in 30-day readmissions.7, 9, 10 A patient navigator intervention in a public safety-net system had differential effects across age groups—19% reduction in hospital encounters among patients age ≥ 60, but 32% increase among patients age < 60—within 180 days of inpatient discharge.11
Several transitional care interventions have reduced 30-day inpatient readmissions,8, 12, 13 and a meta-analysis found greater effects in interventions with many components, involving more individuals in care delivery, or supporting patient capacity for self-care.14 However, the strength of evidence is low because of heterogeneity in interventions, patient populations, clinical settings, and implementation strategies.15 Additionally, 30-day follow-up has limited utility as an indicator of hospital quality,16, 17 and the costs associated with an initial inpatient stay may extend beyond 30 days,18, 19 suggesting a need for evaluating longer-term effects of transitional care interventions.
In this context, we conducted a pragmatic comparative effectiveness trial of a transitional care practice that serves high-risk adults following discharge from a tertiary care academic medical center. Our primary objective was to examine practice effects on the probability of death or additional hospital encounters within 90 days. Our secondary objectives were to examine practice effects on (A) probability of additional hospital encounters within 30 and 180 days, (B) rates of hospital utilization, and (C) patient-reported outcomes.
METHODS
Study Design and Setting
This study was a pragmatic, randomized comparative effectiveness trial that evaluated different forms of post-discharge care after initial discharge from Northwestern Memorial Hospital in Chicago, IL. A “Routine Care” approach, involving direct referral for follow-up care at a local primary care provider, was compared to offering referral for follow-up care at a transitional care practice (TC) across the street from the discharging hospital. Study protocols are detailed elsewhere20 but described briefly here. Protocols were registered in the National Clinical Trials Registry (NCT03066492) and approved by Northwestern University’s institutional review board with a waiver of informed consent for study inclusion and collection of electronic outcome data.
Study Sample and Randomization
In accordance with published criteria defining pragmatic trials,21 this study randomized virtually all eligible patients with any disease state who were successfully engaged by the hospital’s referral team and met inclusion criteria. Patients were considered eligible for inclusion if they (A) were discharged from a hospital “index visit” (i.e., an emergency department [ED] visit, observation stay, or inpatient admission) and were engaged by the hospital’s discharge referral team, (B) were age ≥ 18, and (C) met one of the following referral criteria: (i) had no usual source of care or (ii) expressed that they were unwilling or unable to return to their usual source of care, or their usual care source was insufficient to manage their needs. There were no exclusions based on patients’ language. Patients with a new cancer diagnosis were excluded from randomization but offered full access to the TC practice outside the trial.
The hospital’s discharge referral team, which connects patients with post-discharge care as part of standard hospital workflows—i.e., this team’s clinical tasks had been implemented prior to this pragmatic trial, and no new staff were hired to conduct study recruitment—assessed patients for trial eligibility within existing hospital protocols. Among patients discharged from the ED, referral team staff contacted patients on a drop-in basis, based on factors such as daily staffing levels and timing of ED discharge. Among patients discharged from an observation or inpatient stay, referral team staff contacted all patients whose acute care provider had placed an order for a post-discharge follow-up appointment (of any type). When referral team staff confirmed that a patient met inclusion criteria, they entered an order for TC follow-up care into the electronic health record, which cued a randomization program that allocated the patient to the TC or Routine Care study arm. Although hospital staff and TC providers were not blinded to patients’ study arm assignment, patients were not informed that their post-discharge care instructions involved randomization.
Interventions
The Routine Care intervention consisted of assistance scheduling a post-discharge appointment at a primary care provider that was often a partner of the Northwestern Medicine system. Uninsured patients were referred to an FQHC that partnered with Northwestern Medicine or another FQHC that was convenient for the patient (based on factors such as patient preferences and FQHC location/patient address).
The TC intervention included a scheduled TC practice appointment within 10 days of index visit discharge. The practice offers multidisciplinary, team-based services to foster brief intensive interactions to stabilize medical and psychosocial issues, create positive behavior change, and empower patients to better manage their conditions. TC team members include a medical director, physician (staff and/or trainee), physician assistant, advanced practice nurse, social worker, pharmacist, registered nurse, and a medical assistant. Based on individuals’ psychosocial needs, most patients also received support from a health advocate case manager, and many were seen by a psychiatrist and/or psychologist. There are TC team members in every clinical role who are bilingual English/Spanish speakers.
The TC practice’s care model includes three phases: assessment, intervention, and launch. The initial appointment consisted of comprehensive psychosocial and medical assessments to identify barriers to care and systematically address modifiable barriers.20 At the beginning of the initial TC appointment, a social work assessment screened for insurance status, housing instability, food insecurity, ability to pay for medications and medical expenses, transportation barriers, social supports, mental illness history, and education level.
Following assessment, identified needs were addressed using patient-centered, individually tailored care plans. Common interventions included motivational interviewing to improve adherence with the care plan, connection to state and federal entitlements, simplification of medication regimens and pill box loading, referral to onsite behavioral health therapy or psychiatric evaluation, needs-based health education, transportation coordination, family or support service coordination, specialty care coordination, dietary education, lab testing or medical testing, and wound care. Patients who screened positive for depression or anxiety, reported a history of trauma, or requested substance abuse or behavioral health services were offered therapy, psychiatry, or connection to community substance abuse treatment. Follow-up appointments at the TC practice were scheduled as needed, with most patients initially seen weekly for medication management, assistance with insurance applications, and self-management support.
When the patient and care team determined the patient was ready to receive care from a community-based primary care provider, a health advocate scheduled an appointment within 14 days with a provider (typically at an FQHC) who would become the patient’s new source of primary care. The TC care team deemed patients ready to “launch” from the practice after they met criteria including patient education through “teach-back” for multiple knowledge domains—such as addressing transportation barriers for community-based appointments, and documentation required to receive financial discounts at scheduled primary care appointments—and implementation of a sustainable medication regimen.20 At the time of launch, patients were also offered ongoing access to specialty care within the Northwestern Medicine system.
Data Collection and Measures
A study programmer queried health system databases to collect data on patients’ index visits and sociodemographic characteristics. Based on published predictive models of risk factors that predict hospital encounters after initial discharge, we also collected variables on inpatient admissions during the prior year,22,23,24 emergency/observation encounters during the prior 6 months,24 and index visit length of stay.23 Patients’ addresses were linked with 2015 American Community Survey25 data to construct census tract-level measures of residential poverty using a previously published definition of high-poverty areas.26, 27 Deaths during study follow-up were confirmed by linkage with National Death Index (NDI) records.28
This trial’s primary outcome was a binary indicator of death or any additional hospital encounters—i.e., one or more ED visit, observation stay, or inpatient admission—within 90 days of index visit discharge. Secondary outcomes included binary indicators of additional hospital encounters within 30 days and 180 days of discharge, and four count outcomes for the 30-day, 90-day, and 180-day periods following discharge: (1) ED visits, (2) observation stays, (3) inpatient admissions, and (4) total hospital encounters (sum of ED, observation, and inpatient).
Approximately 90 days after discharge, bilingual English/Spanish speaking study staff phoned each patient up to four times to collect survey data. Surveys assessed overall health status, summary scores of physical and mental health,29, 30 and patient activation.31, 32 Medical Expenditure Panel Survey items assessed whether patients had a usual source of care, and self-reported ED visits and hospital admissions since initial discharge.33 Participants provided verbal informed consent and received a $25 gift card for survey completion. Results were entered in REDCap software.34
Sample Size
This trial was designed to test whether, among patients attending any scheduled TC appointments, the TC intervention could reduce the proportion with any additional hospital encounters over 90 days to ≤ 25%. Based on internal analyses of administrative data, we estimated that 45% of patients offered post-discharge TC care would attend their scheduled follow-up appointment. We assumed a 55% event rate for both patients who were offered Routine Care and the subgroup of those offered TC care who did not attend any appointments, which yielded a projected 42% overall event rate in the TC arm. Based on eligible patient discharge volumes and TC practice capacity, randomization was designed with a 3:1 allocation ratio (i.e., 75% randomized to TC). Using a two-sided χ2 test of dichotomous proportions with α = 0.05, a sample size of 490 patients randomized to TC care and 164 to Routine Care (total N = 654) provided 80% power to detect this difference.
Statistical Analysis
We conducted multivariable regression analyses for all utilization outcomes based on the intention-to-treat principle. For the primary outcome, we estimated a Poisson regression model with robust variance,35 which produced an adjusted relative risk (RR). For secondary outcomes, we estimated Poisson models with robust variance for binary outcomes, and negative binomial models for count outcomes. We calculated predictive margins using Stata’s “margins” command, with proportions (binary outcomes) or rates (count outcomes) adjusted across the sample’s covariate distribution. All regression models adjusted for age (continuous), sex, insurance (public, private, uninsured), race/ethnicity, homelessness, index visit type, index visit length of stay, prior ED/observation visits, and prior inpatient admissions. Count regressions accounted for censoring due to death with an exposure term for days of follow-up while alive.
We analyzed telephone survey results using t tests for means, chi-square tests for unordered categorical variables, and Wilcoxon rank-sum tests for ordered categorical variables (all two-sided tests with α = 0.05). Analyses were conducted using Stata, version 14.2 (StataCorp; College Station, TX).
RESULTS
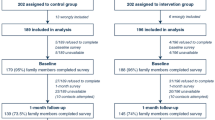
Study enrollment began in September 2015 and concluded in February 2016. During this period, 45,656 unique patients were discharged from Northwestern Memorial Hospital after an ED visit, observation stay or inpatient admission (Fig. 1). A total of 12,770 patients were engaged by the discharge referral team, and 654 eligible patients were identified for randomization; 490 were randomized to TC referral and 164 to Routine Care. Among randomized patients, 285 (43.6%) were inpatient discharges (Table 1), with 211 of 285 (74.0%) discharged from inpatient general medicine service lines, 29 (10.2%) from medical specialty service lines, and 45 (15.8%) from other inpatient service lines. In the entire sample (N = 654), the most common primary discharge diagnoses from index visits were chest pain/angina (7.4%), trauma (7.1%), abdominal pain (6.6%), other gastrointestinal (4.8%), cellulitis/wound/infectious (4.6%), and other infectious disease (4.6%).20
At the time of index visit discharge, included patients had a mean age of 43.8 years, and 41.4% were female (Table 1). The most common racial/ethnic group in this diverse study sample was Black/African-American (30.1%). About half (49.7%) of patients had Medicaid insurance, and about one third (34.6%) were uninsured. Among patients with valid address information, 57.4% were either homeless or lived in a high-poverty census tract. Due to random chance, Routine Care patients were more likely to have index visit length of stay exceeding 48 h (56.1% versus 45.5%), and the trial arms differed in the numbers of ED visits/observation stays (prior 180 days) and inpatient admissions (prior year) preceding the index visit.
As we anticipated, many patients in the TC arm did not attend any follow-up appointments at the TC; 176 (35.9%) patients attended any TC visits within 30 days post-discharge, and 184 (37.6%) attended any visits within 180 days. The median time to first visit was 6 days (interquartile range [IQR] 4–9). Within the TC arm, TC “attenders” were more often female (47.8% versus 37.6% for those with no visits; P = 0.03) and less often homeless (1.6% versus 9.2%; P = 0.001). At 90 days, attenders had a mean of 3.2 (SD 2.8) and median of 2 (IQR 1–4) visits. At 180 days, attenders had a mean of 4.0 (SD 4.1) and median of 2 (IQR 1–5.5) visits.
Due to the pragmatic nature of our randomization, 9 patients in the Routine Care arm (5.5%) attended any TC visits after the patient or hospital provider requested an appointment. These patients were analyzed according to the intent-to-treat principle.
Hospital Use Results
In multivariable regression analysis of our primary outcome, there was no statistically significant difference between arms in the probability of death or additional hospital encounters (ED, observation, or inpatient) within 90 days (RR 0.91; 95% confidence interval [CI] 0.74–1.13) (Table 2).
In multivariable analysis of secondary outcomes, there were no significant differences in probabilities of each hospital encounter type at 30 days post-discharge (Table 2). However, in the TC arm, there was 37% reduced probability of any inpatient admission over 90 days (RR 0.63; 95% CI 0.43–0.91), and 35% reduced probability of any inpatient admission over 180 days (RR 0.65; 95% CI 0.47–0.89). Over 180 days, the adjusted proportion of patients with any inpatient admission was 23.1% in the Routine Care arm and 15.0% in the TC arm.
Over 30 days and 90 days, there were no significant differences in hospital encounter utilization rates (Table 3). However, over 180 days, TC patients had 42% fewer inpatient admissions (incidence rate ratio 0.58; 95% CI 0.37–0.90); the adjusted 180-day rate of inpatient admissions was 52.5 per 100 patients in the Routine Care arm and 30.5 per 100 patients in the TC arm.
Telephone Survey Results
The follow-up telephone survey was completed by 115 patients (17.6%); 94 TC patients (19.2%) completed the survey, versus 21 (12.8%) for Routine Care (P = 0.063). Survey completion differed by race/ethnicity (P < 0.001), with participation highest among Hispanic/Latino patients (30.6%). TC patients were less likely to report any inpatient admission since the index visit (6.7% versus 30.8%; P = 0.01) or a usual source of care (61.7% versus 85.7%; P = 0.04). There were no significant differences between arms in self-rated health, ED visits, or patient activation.
DISCUSSION
In this pragmatic comparative effectiveness trial, the TC intervention did not cause a significant reduction in the 90-day probability of death or additional hospital encounters. However, there were significant reductions in key secondary measures of inpatient utilization. Patients in the TC arm had 42% fewer inpatient admissions over 180 days and were at least 35% less likely to have any inpatient admission at 90 and 180 days. While most TC practice visits occurred within 90 days, effects on inpatient outcomes either achieved statistical significance (rate of admissions) or remained significant (any admissions) as the length of follow-up extended from 90 to 180 days.
Multiple factors could have contributed to the TC intervention’s effects on inpatient admissions. In accordance with prior meta-analysis findings,14 the TC intervention had multiple components, several individuals involved in care delivery, and attempted to improve patients’ capacity for self-care. However, whereas the TC intervention occurred entirely post-discharge, multiple interventions that have reduced 30-day rehospitalizations also had pre-discharge components.36, 37 Jack et al. reduced 30-day rehospitalizations in safety-net hospital patients through an intervention with pre-discharge nurse components and post-discharge clinical pharmacist follow-up.8 More explicit integration of the TC practice with pre-discharge transitional care could lead to increased practice attendance and, in turn, increased intervention effects.
The TC practice’s care model seems well-suited to its relatively young patient population (84% of study sample under age 60) that was diverse with regard to both SES and race/ethnicity. Our findings contrast with a prior patient navigator trial in a safety-net health system, where patients under age 60 had 32% more hospital encounters at both 30 days9 and 180 days.11 In that prior patient navigator intervention, community health workers made one hospital encounter and three post-discharge outreach calls.9 In contrast, the TC care team tailored care delivery to address each patient’s critical medical and psychosocial needs. Also, the TC intervention seems to confer benefits beyond the period when patients attend follow-up practice visits, and aligns with prior evidence of the effectiveness of complex and supportive strategies for reducing readmissions.14
Our study has several limitations. First, we were unable to discriminate avoidable from “planned” readmissions, which might have introduced unavoidable events in both trial arms. Second, observed event rates were lower than historic rates used in statistical power calculations, which effectively reduced our ability to detect modest differences between arms. Third, an important limitation is that outcome data were from a single institution, and some patients may have visited other regional hospitals. However, it is likely that ongoing TC support would increase patients’ likelihood of returning to the institution where their index visit occurred. Therefore, our results could understate intervention effects, and future research should comprehensively assess regional post-discharge hospital use. Fourth, despite our randomization, study arms were imbalanced on some prognostic factors. Had we not adjusted for these factors in multivariable regression analyses, we would have overestimated the TC’s ability to reduce subsequent hospital use. Fifth, due to our use of existing institutional data within this pragmatic trial,21 we could not comprehensively assess patients’ comorbidities at baseline and we could only assess neighborhood-level income. Nevertheless, the variety of index visit diagnoses in the study sample,20 in combination with statistically significant intervention effects, seem to demonstrate how the TC intervention optimized care transitions through a broad, patient-centered approach.
At the time of this study, the TC had been operating for 4 years and had refined staffing and protocols to fit its patient population; it may be unreasonable to assume that a similar practice at another institution could immediately achieve results observed here. Additionally, the TC practice served a highly selective patient population that lacked a trusted usual source of care and were predominantly uninsured or had Medicaid. We cannot speculate on intervention effects in other populations.
In summary, in a pragmatic comparative effectiveness trial of a post-discharge transitional care practice serving a vulnerable, high-risk population, there were significant reductions in measures of inpatient admissions at 90 days and 180 days.
References
Lee KK, Yang J, Hernandez AF, Steimle AE, Go AS. Post-discharge Follow-up Characteristics Associated With 30-Day Readmission After Heart Failure Hospitalization. Med Care 2016;54(4):365–372.
Gold HT, Slover JD, Joo L, Bosco J, Iorio R, Oh C. Association of Depression With 90-Day Hospital Readmission After Total Joint Arthroplasty. J Arthroplast 2016;31(11):2385–2388.
Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 2003;51(4):549–555.
Burke RE, Guo R, Prochazka AV, Misky GJ. Identifying keys to success in reducing readmissions using the ideal transitions in care framework. BMC Health Serv Res 2014;14:423.
Kangovi S, Barg FK, Carter T, et al. Challenges faced by patients with low socioeconomic status during the post-hospital transition. J Gen Intern Med 2014;29(2):283–289.
Kangovi S, Levy K, Barg FK, Carter T, Long JA, Grande D. Perspectives of older adults of low socioeconomic status on the post-hospital transition. J Health Care Poor Underserved 2014;25(2):746–756.
Englander H, Michaels L, Chan B, Kansagara D. The care transitions innovation (C-TraIn) for socioeconomically disadvantaged adults: results of a cluster randomized controlled trial. J Gen Intern Med 2014;29(11):1460–1467.
Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med 2009;150(3):178–187.
Balaban RB, Galbraith AA, Burns ME, Vialle-Valentin CE, Larochelle MR, Ross-Degnan D. A Patient Navigator Intervention to Reduce Hospital Readmissions among High-Risk Safety-Net Patients: A Randomized Controlled Trial. J Gen Intern Med 2015;30(7):907–915.
Kangovi S, Mitra N, Grande D, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Intern Med 2014;174(4):535–543.
Balaban RB, Zhang F, Vialle-Valentin CE, et al. Impact of a Patient Navigator Program on Hospital-Based and Outpatient Utilization Over 180 Days in a Safety-Net Health System. J Gen Intern Med 2017:1–9.
Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med 2006;166(17):1822–1828.
Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281(7):613–620.
Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med 2014;174(7):1095–1107.
Kansagara D, Chiovaro JC, Kagen D, et al. So many options, where do we start? An overview of the care transitions literature. J Hosp Med 2016;11(3):221–230.
Kociol RD, Liang L, Hernandez AF, et al. Are we targeting the right metric for heart failure? Comparison of hospital 30-day readmission rates and total episode of care inpatient days. Am Heart J 2013;165(6):987–994 e981.
Chin DL, Bang H, Manickam RN, Romano PS. Rethinking Thirty-Day Hospital Readmissions: Shorter Intervals Might Be Better Indicators Of Quality Of Care. Health Aff (Millwood) 2016;35(10):1867–1875.
Chandra A, Dalton MA, Holmes J. Large increases in spending on postacute care in Medicare point to the potential for cost savings in these settings. Health Aff (Millwood) 2013;32(5):864–872.
Likosky DS, Zhou W, Malenka DJ, Borden WB, Nallamothu BK, Skinner JS. Growth in medicare expenditures for patients with acute myocardial infarction: a comparison of 1998 through 1999 and 2008. JAMA Intern Med 2013;173(22):2055–2061.
Schaeffer C, Teter C, Finch EA, et al. A pragmatic randomized comparative effectiveness trial of transitional care for a socioeconomically diverse population: Design, rationale and baseline characteristics. Contemp Clin Trials 2018;65:53–60.
Thorpe KE, Zwarenstein M, Oxman AD, et al. A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. J Clin Epidemiol 2009;62(5):464–475.
Donze J, Aujesky D, Williams D, Schnipper JL. Potentially avoidable 30-day hospital readmissions in medical patients: derivation and validation of a prediction model. JAMA Intern Med 2013;173(8):632–638.
Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med 2010;25(3):211–219.
van Walraven C, Wong J, Forster AJ. LACE+ index: extension of a validated index to predict early death or urgent readmission after hospital discharge using administrative data. Open Med 2012;6(3):e80–90.
United States Census Bureau. American Community Survey Data Releases. https://www.census.gov/programs-surveys/acs/news/data-releases.2015.html. Accessed 20 March 2019.
Bishaw A. Areas with concentrated poverty: 2006–2010. American Community Survey Briefs, Vol 9: US Department of Commerce, Economics and Statistics Administration, United States Census Bureau; 2011.
Jiang Y, Novais AP, Viner-Brown S, Fine M. Non-emergent hospital emergency department use and neighborhood poverty in Rhode Island 2008-2012. RI Med J 2014;97(7):47–51.
Centers for Disease Control and Prevention. National Death Index. 2017. https://www.cdc.gov/nchs/ndi/index.htm. Accessed 20 March 2019.
Maruish MEE. User’s manual for the SF-12v2 Health Survey (3rd ed.). Lincoln, RI: QualityMetric Incorporated; 2012.
Cheak-Zamora NC, Wyrwich KW, McBride TD. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Qual Life Res Int J Qual Life Asp Treat Care Rehab 2009;18(6):727–735.
Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res 2005;40(6 Pt 1):1918–1930.
Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39(4 Pt 1):1005–1026.
Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. 2004. https://meps.ahrq.gov/mepsweb/survey_comp/survey_results_ques_sections.jsp?Section=AC&Year1=2004&Submit1=Search. Accessed 20 March 2019.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–381.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159(7):702–706.
Rennke S, Nguyen OK, Shoeb MH, Magan Y, Wachter RM, Ranji SR. Hospital-initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med 2013;158(5 Pt 2):433–440.
Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med 2011;155(8):520–528.
Acknowledgments
We thank the patients who participated in this study, along with care team members and staff at the Northwestern Medical Group Transitional Care practice. We thank the Chicago-area FQHCs that provided care to patients in both study arms and AllianceChicago for collaboration in data acquisition efforts. We also recognize the support and participation of Northwestern Memorial HealthCare and providers and staff at Northwestern Memorial Hospital. We thank Dyanna Gregory, MS, who led early work on several aspects of study randomization and analysis, and Michelle Cates and Mya Carter, who conducted follow-up phone interviews.
Funding
This research was supported by funding from Northwestern Memorial Hospital and the J.B. and M.K. Pritzker Family Foundation. Funders were not involved in reviewing or approving the manuscript for publication. REDCap is supported at Feinberg School of Medicine by the Northwestern University Clinical and Translational Science (NUCATS) Institute. Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences (#UL1TR001422).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Protocols were registered in the National Clinical Trials Registry (NCT03066492) and approved by Northwestern University’s institutional review board with a waiver of informed consent for study inclusion and collection of electronic outcome data.
Conflict of Interest
Dr. Schaeffer, Ms. Rogers, and Ms. Teter report employment as health care providers at the Northwestern Medical Group Transitional Care (TC) practice, and Ms. Hurt formerly provided social work services at the Northwestern Medical Group TC practice. All remaining authors declare that they do not have a conflict of interest.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liss, D.T., Ackermann, R.T., Cooper, A. et al. Effects of a Transitional Care Practice for a Vulnerable Population: a Pragmatic, Randomized Comparative Effectiveness Trial. J GEN INTERN MED 34, 1758–1765 (2019). https://doi.org/10.1007/s11606-019-05078-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-05078-4